Effective pain management is an immense challenge for researchers, clinicians, and especially those who suffer from it. Many treatment options exist, but each carries its own risk. For example, opioids can be highly effective, but extended use can impair sleep and misuse can be fatal. On the other hand, ‘alternative’ therapies like chiropractic manipulation and acupuncture carry little to no risk, but are not consistently effective for some patients.
Clearly, more research needs to be done to better understand how different conditions cause pain and how to effectively treat it. The three publications below look at pain in disparate contexts: migraine, neuropathic pain and oral cancer. They do share a common thread, though – all three use our 300C-I Mechanical Stimulator to quantify mechanosensitivity.
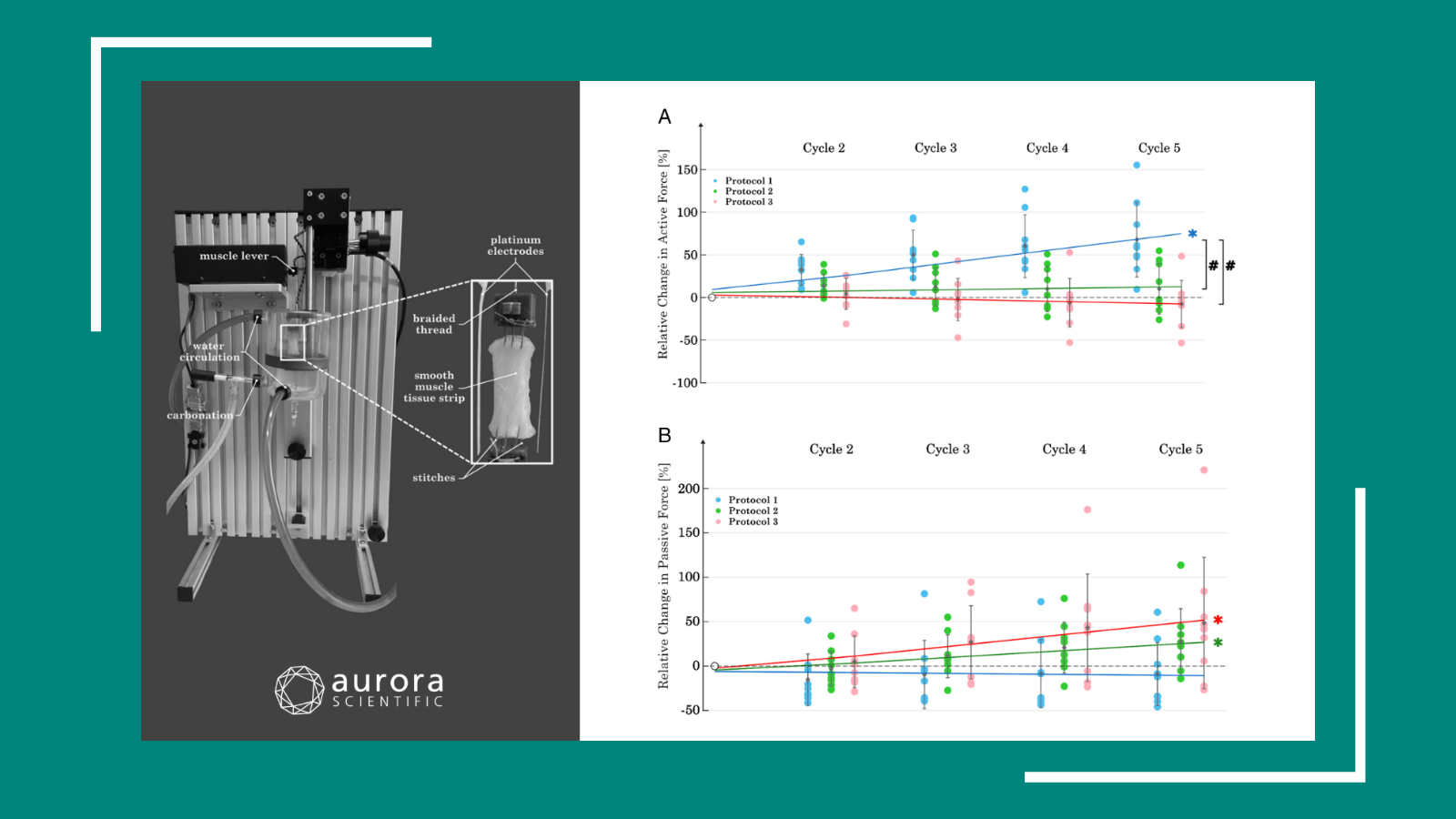
Dissociation between CSD-Evoked Metabolic Perturbations and Meningeal Afferent Activation and Sensitization: Implications for Mechanisms of Migraine Headache Onset
Migraine headache is more prevalent than you might imagine – it’s the second leading cause of disability in the world. The onset of the headache phase requires both the activation and increased mechanosensitivity of the afferent neurons that innervate the intracranial meninges. For migraine with aura (a common subtype of migraine), activation and sensitization follow cortical spreading depression (CSD), a wave of depolarization that spreads across the cortex. However, the mechanisms by which CSD activates and sensitizes the meningeal afferents is not known.
In this study, the Zhao and Levy set out to determine whether cortical hypoperfusion and decreased tissue oxygenation following CSD contribute to meningeal nociception in anesthetized rats. After identifying the target meningeal afferents, the researchers applied stimuli using an Aurora Scientific Dual-Mode Indenter. Responses to the mechanical stimuli were measured via continuous electrophysiology. The researchers induced CSD by inserting a micropipette into the frontal cortex, then immediately measured perfusion and cortical partial pressure of oxygen.
Using naproxen (a cyclooxegenase inhibitor) to prevent CSD-induced hypoperfusion and reduction in tpO2, they found that mechanosensitization of afferents was blocked, but did not reduce activation. On the other hand, using Levcromakalim (a vasodilator that functions independently from cyclooxegenase) to counteract the hypoperfusion, activation of afferents was blocked, while sensitization was unaffected.
The authors conclude that there are
“distinct mechanisms underlying the activation and sensitization of meningeal afferents in migraine, and highlight the need to target both processes for an effective migraine therapy”.
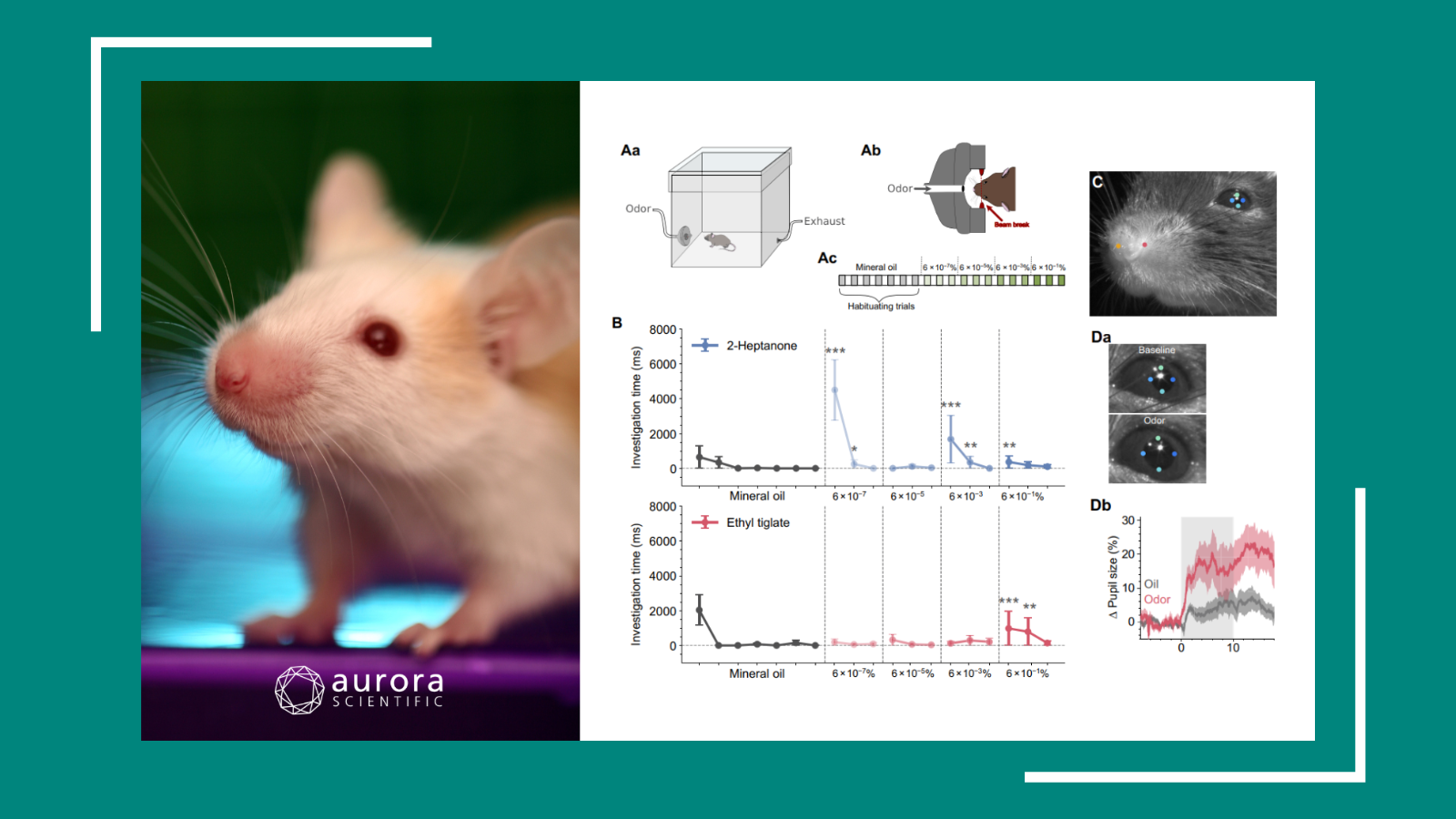
Modulation of SUR1 KATP Channel Subunit Activity in the Peripheral Nervous System Reduces Mechanical Hyperalgesia after Nerve Injury in Mice
Another highly prevalent condition, neuropathic pain affects at least 6% of the general population, but some estimates have gone as high as 17%. Many of our current treatments are ineffective, so there is a great need to develop improved therapies. It is clear that ATP-sensitive potassium channels play a critical role in modulating the excitation of neurons, but the roles of some KATP subunits during chronic pain are not fully understood.
In this study, the Luu, et al. looked at the role of two genes thought to be involved in chronic pain in mice. In particular, they were interested in the genes encoding Kir6.2 and SUR1, which are involved in the formation and regulation of potassium channels, respectively.
To do this, they induced chronic pain via spinal nerve ligation and assessed mechanical sensitivity by assessing paw withdrawal thresholds. They found that expression of SUR1 and Kir6.2 was reduced more than 30 days after spinal nerve ligation. Using two genetic models—global SUR1 knockout and knockdown of SUR1 using shRNA—they found that mice lacking SUR1 had mechanical hypersensitivity. They also assessed pharmacological treatments, and found that administration of potassium channel agonists greatly reduced mechanical sensitivity. In ex vivo electrophysiology tests, administration of potassium channel agonists reduced potentials evoked in single nerve fibers following mechanical stimulation using the Aurora Scientific 305C-I mechanical stimulator.
In conclusion, the authors write that,
“Potassium channels present a target for analgesic therapies, especially since they are expressed in nociceptors and could play an essential role in regulating the excitability of neurons involved in pain-transmission.”
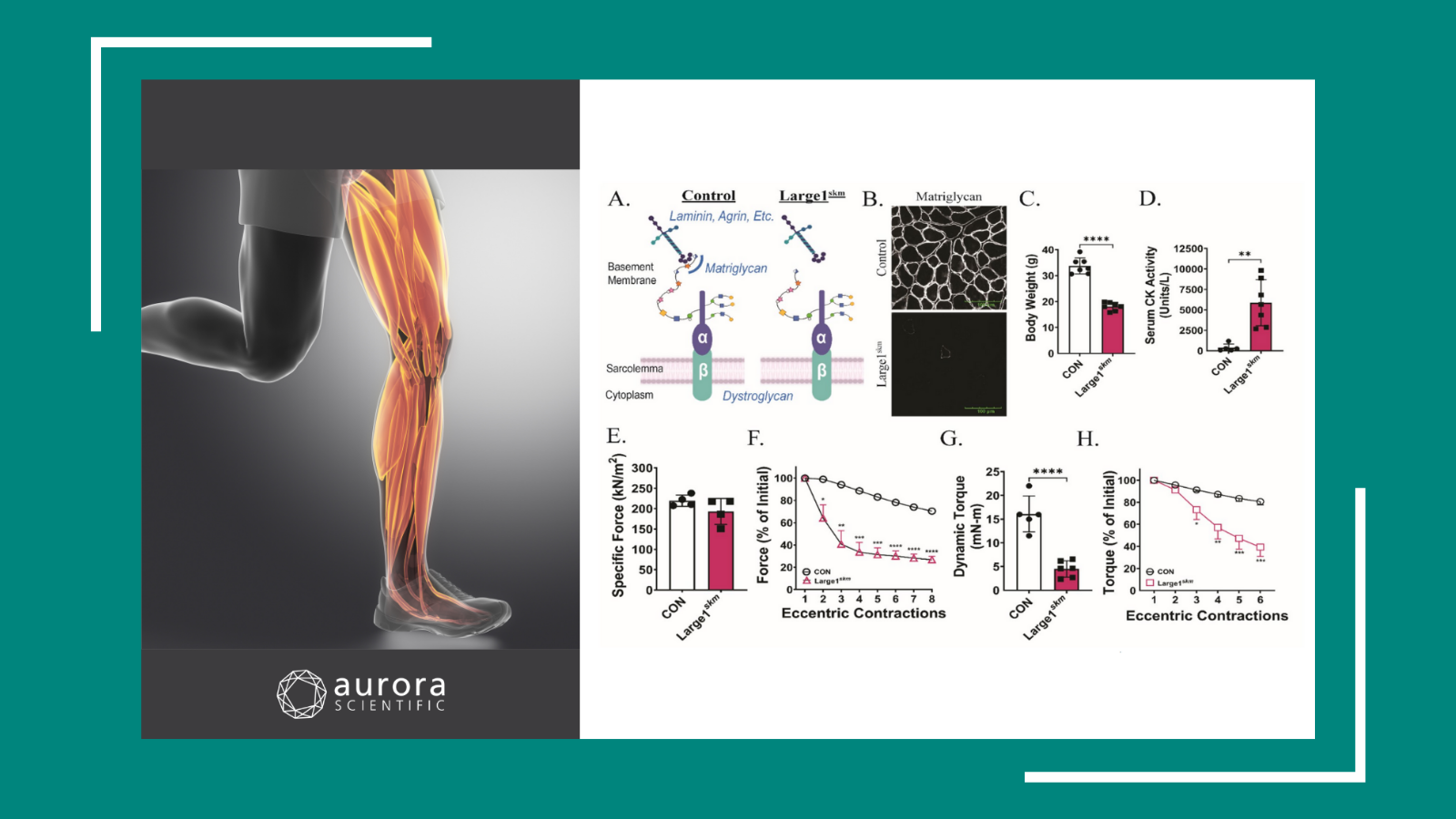
Depiction of Oral Tumor-Induced Trigeminal Afferent Responses Using Single-Fiber Electrophysiology
Among cancers, oral cancer is unique in that pain is often the first symptom. Opiates are frequently prescribed, but addiction and drug tolerance can add to the significant personal burden of cancer. Currently, the mechanisms by which oral cancer modulates nerves to produce pain are unclear.
In this study, Grayson et. al. describe a novel ex vivo method to record the activity of single neurons in the lingual nerve, and how they used this protocol to study how nerve terminals are sensitized in a murine model of squamous cell carcinoma.
First, they discuss their method to dissect the tongue, isolate individual nerve filaments and record neural activity. They identified receptive fields using electrical stimulation, then assessed the mechanical sensitivity of individual fibers using an Aurora Scientific 300-series Dual-Mode mechanical stimulator to apply a series of ascending stimuli to the most sensitive area of the receptive field.
In both control and tumour-bearing tissue, they found that a fraction of fibers were mechanically insensitive. However, tumour-bearing tissue had a significantly smaller fraction of these insensitive fibers. Similarly, the occurrence of spontaneously active fibers and the discharge rate of continuously active fibers were significantly higher for the cancer-bearing preparations. Using mechanical stimulation, they found that tongue tumour lowered mechanosensitivity thresholds and increased the firing rates of some afferents.
These findings mirror symptoms reported in the clinic: both sudden pain and hypersensitivity are frequently reported by patients with oral cancer. The authors note that this is the first study to use ex vivo single-fiber recordings of trigeminal afferents to assess oral cancer-nerve interactions. They conclude,
“Single-fiber recordings of the different lingual afferents will offer increased insight into peripheral mechanisms of oral cancer-induced pain as well as serve as a platform to test for analgesic drugs to treat cancer pain.”